Image Source: Unsplash.com
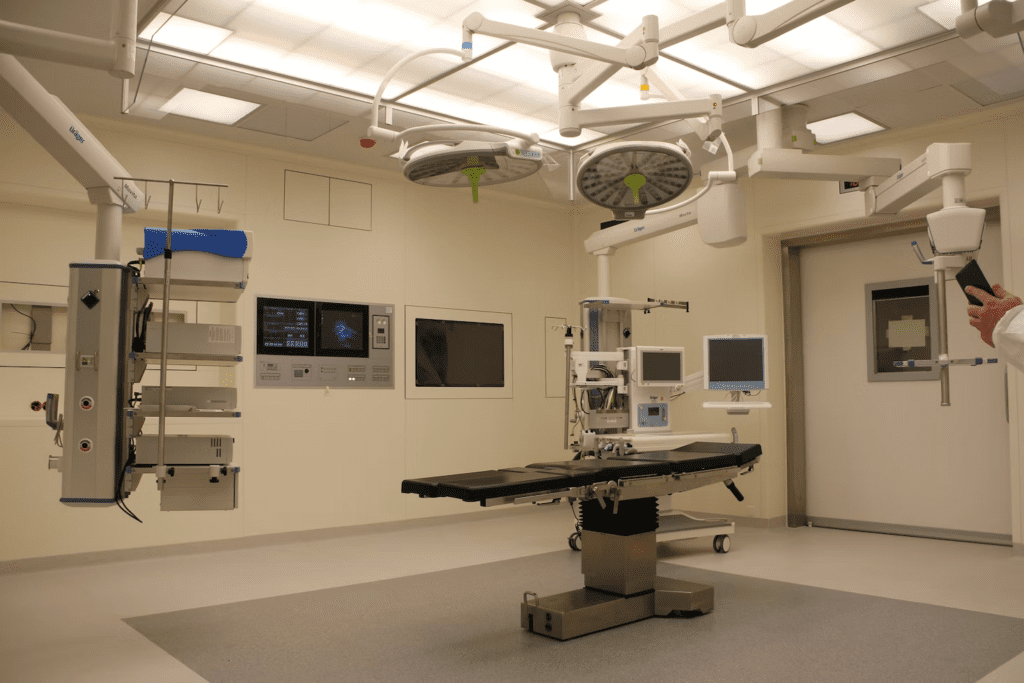
Someone is transforming Mars into a self-sufficient city in 20 years. It would be a sin not to use such echelons of technology in today’s healthcare. From the looks of it, we’re long past getting started. From robotic surgeries to 3D-printed human organs, we are undeniably in the zone in 2022. Even the US FDA seems to agree.
According to the agency, health tool digitization can revolutionize accuracy in medical diagnosis, treatment, and overall healthcare delivery. The only problem is it’s not as seamless as it sounds.
Over 80,000 deaths and 1.7 million injuries resulted from medical device-related errors in the last ten years. Funny how these numbers also come from the FDA.
So are medical technologies increasing the risk of medical errors? Are they a boon or bane for public health? No one seems to have the answers yet. But we know that recent developments are changing people’s minds about the actual status quo with healthcare digitization. Let’s look into why.
4 Digital Health Technologies Known To Cause Medical Errors
Humans don’t come anywhere near machines in terms of precision. Apparently, it doesn’t always work that way in healthcare. Here are four common applications of digital medical technology and the reasons healthcare organizations must adopt them with caution.
Electronic Health Records (EHRs)
The wisdom of EMRs lies in making patient health information more accessible to healthcare professionals and organizations. Like many other digital technologies, their goal is to increase efficiency, but this doesn’t always translate to effectiveness.
In a University of Utah study, EMRs failed to identify as much as 33% of possible adverse drug interactions and other medication errors. Then, of course, there’s a whole plethora of factors behind EHR errors, from alert fatigue to fatigued practitioners, etc.
Infusion pumps
Infusion pumps, also known as smart pumps, are digital machines that deposit nutrition or medication directly into the bloodstream. Because of their design, even the tiniest errors can be gravely harmful, even fatal.
Infusion pump problems can arise from human lapses, such as entering the wrong medication or the wrong infusion rate. Otherwise, the culprit could be a technical issue, like improperly charged batteries or electromagnetic interference (for example, from a mobile phone).
In the U.S., 7,000 to 9,000 patients die yearly due to medication errors. Considering 87% of hospitals in the country use smart pumps, it’s hard not to see a significant correlation. This prompted many victims to reach out to personal injury law firms to help them assess the case so they can file a claim for damages.
Medical AIs
Healthcare Artificial Intelligence (AI) now ranges from surgical robots to virtual assistants answering queries from patients, if not diagnosing them altogether. Again, while AIs couldn’t sound more perfect in theory, even they seem to work differently in real life.
The issue with medical AI is not only that they’re not ready to act with complete autonomy. The “black box” problem” also keeps them from receiving the necessary human intervention. While these machines can work on human-fed “reasoning” methods and algorithms, they can’t thoroughly explain their conclusions in human terms,
This can be particularly critical in disease detection. Medical professionals might never realistically cover all bases when verifying AI diagnoses, which puts patients at risk.
Medical AIs are not safe from technical errors either. If a bug attacks surgical robot software, for example, the AI can malfunction during surgery and endanger the patient. During a cyberattack, a hacker can quickly turn the robot into anything, including a weapon.
Medical 3D printing
Medical 3D printing is the process of producing exact replicas of anatomical structures using additive manufacturing technology. Examples of devices created using this technology are orthopedic implants and prostheses.
By the end of 2028, experts project a 15.4% CAGR for the industry and USD 6.78 billion in revenues. In yet another perfect-world scenario, the benefits of medical 3D printing are endless until you consider the risks.
For one, the process releases ultrafine dust that carries human hazards like cell injury and inflammation. Like air pollution from vehicular exhaust, these microscopic particles can cause lung and heart disease when regularly inhaled.
The most significant danger, however, is the considerable knowledge gap in the materials, methods, and finishing processes of additive manufacturing. Throwing in a 3D medical printer among brilliant and dedicated doctors in a hospital doesn’t make it heaven-sent.
When untrained people print medical devices with a 3D printer, patients can suffer infections, stalled medical procedures, and surgical complications.
Why Medical Errors Still Occur With High-Tech Medical Devices
When it comes to medical errors, there will always be that crack in the door in a hospital of humans. With digital machines, our expectations are higher. So why are medical device errors still an alarming cause of severe injuries and deaths despite massive healthcare digitization?
The reasons are many – no proper manufacturer testing, contamination, stress overload, inadequate maintenance and care, etc. The irony is that human errors are also on the list and way up there. As much as 90% of medical errors are due to human lapses, both with devices and in general.
The Trap of Human Frailty: Balancing Benefits and Risk
It seems our human limits will get the best of us wherever we go. But we’ve come so far in digitizing healthcare, and we need to go beyond the boon-or-bane analysis to move forward.
It might be time to stop asking whether technology increases the risk of medical errors. Instead, let’s assess what we can do and ensure that we’re tipping the balance in our favor.
We could design more human-centric devices and develop a stronger knowledge base among health professionals as users. Healthcare specialists and device manufacturers can collaborate more. Healthcare organizations planning to adopt specific technologies can follow a more stringent evaluation process.
Our current system has no solid reporting process for the performance and failure of medical equipment. Let’s have one, along with stricter FDA regulations. Anyone responsible for medical blunders, with or without devices, should also be held accountable. And, of course, patients suffering from medical malpractice must have the whole nine yards of the law to protect them.